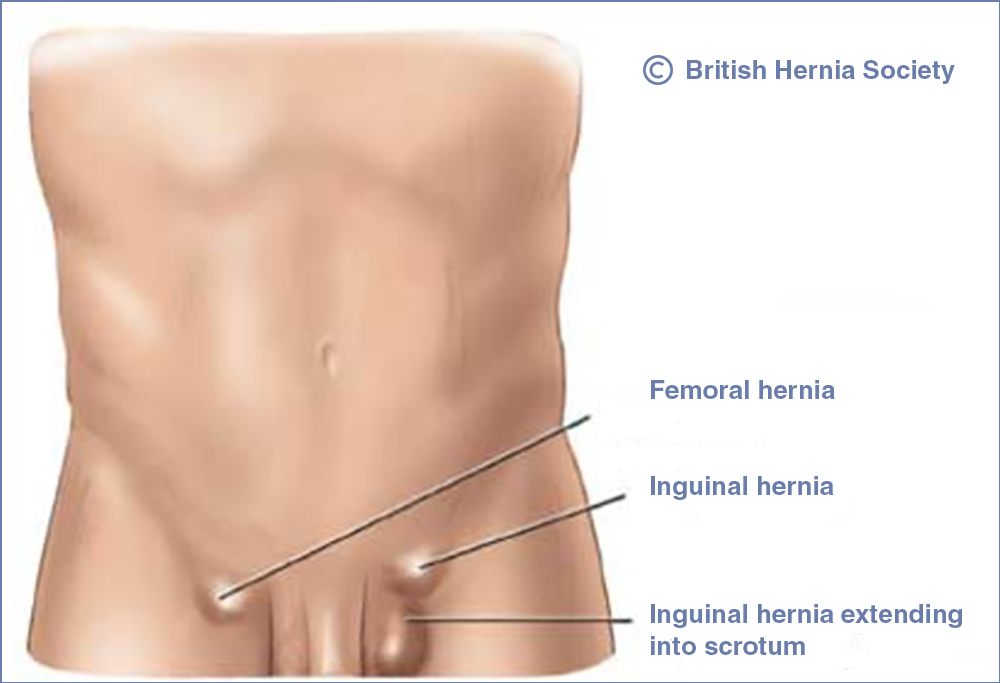
An inguinal hernia is the most common type of hernia. It can appear as a swelling or lump in your groin, or as an enlarged scrotum (the pouch containing the testicles). The swelling may be painful.
The lump often appears when you’re lifting something and disappears when you lie down.
An inguinal hernia usually occurs when fatty tissue or a part of your bowel, such as the intestine, pokes through into your groin at the top of your inner thigh. It pushes through a weak spot in the surrounding muscle wall (the abdominal wall) into an area called the inguinal canal.
Inguinal hernias occur mainly in men. Most are thought to result from ageing, although they can occur at any age. This is because as you get older, the muscles surrounding your abdomen (tummy) can become weaker.
Inguinal hernias can sometimes appear suddenly after putting pressure on the abdomen, such as straining on the toilet if you have constipation or carrying and pushing heavy loads. They have also been linked to having a persistent, heavy cough.
Inguinal hernias can be repaired using surgery to push the bulge back into place and strengthen the weakness in the abdominal wall. The operation is usually recommended if you have a hernia that causes pain, severe or persistent symptoms, or if any serious complications develop.
Surgery gets rid of the hernia to prevent any serious complications, but there’s a chance it could return after the operation.
There are 2 ways an inguinal hernia repair can be performed:
- open surgery – where a cut is made to allow the surgeon to push the lump back into the abdomen
- laparoscopic (keyhole) surgery – a less invasive, but more difficult, technique where several smaller cuts are made, allowing the surgeon to use various special instruments to repair the hernia
There are advantages and disadvantages to both methods. The type of surgery you have depends on which method suits you and your surgeon’s recommendation.
You should be able to go home the same day or the day after surgery. It’s important to follow the hospital’s instructions on how to look after yourself. This includes eating a good diet to avoid constipation, caring for the wound, and not straining yourself too soon. Most people make a full recovery from inguinal hernia repair within 4 weeks, although many people can return to driving, work and light activities within 2 weeks.
Inguinal hernia surgery is most often carried out under general anaesthetic. There are 2 important complications a patient should be aware of:
- Recurrence: hernias can come back no matter how they are repaired. We try to minimise the risk of recurrence by using mesh to reinforce the repair. However, we cannot make the risk zero. It is estimated that the risk of recurrent hernia is ~0.5% in the first 1-3 years, but increases to 5% by 10years and perhaps 10% at 20years. Most surgeons agree that the risk of recurrence would be significantly higher if no mesh were used.
- Chronic groin pain: this is defined as continuous post-operative groin pain lasting 6 months or more after groin hernia repair. This is multifactorial, and we do not know all the reasons that some patients get chronic pain. Most surgeons do not believe that mesh is the only cause of this phenomenon. A large study from the USA suggested the risk of chronic groin pain after open groin hernia repair may be as high as 5-10%. Using keyhole surgery and fixation free mesh reduces that risk.
There are also some other complications that are less troublesome, or much rarer.
These include bruising in the groin of scrotum after repair of large or chronic hernias (this usually settles within 2 weeks).
Some patients with enlarged prostates may struggle to pass water post-operatively, and require a urinary catheter (retention of urine).
Wound or mesh infections are very rare, as is interruption of the blood supply of the testicle.